Understanding the United Health Care prior auth tool is crucial for both patients and healthcare providers. This tool helps ensure that medical procedures and treatments are medically necessary and covered under a patient’s health insurance plan before they are performed. Knowing how to effectively utilize this system can streamline the healthcare process and avoid potential billing surprises.
Understanding the Importance of the United Health Care Prior Auth Tool
The prior authorization process, facilitated by the United Health Care prior auth tool, is a critical step in managing healthcare costs and ensuring patients receive appropriate care. It allows United Health Care to review planned treatments and procedures to confirm their medical necessity and appropriateness based on established clinical guidelines. This process helps to prevent unnecessary or potentially harmful procedures and ensures that the most effective and cost-efficient treatment options are utilized.
How to Use the United Health Care Prior Auth Tool: A Step-by-Step Guide
Navigating the United Health Care prior auth tool can seem daunting at first, but with a clear understanding of the process, it becomes much simpler. Here’s a breakdown of how to effectively use the tool:
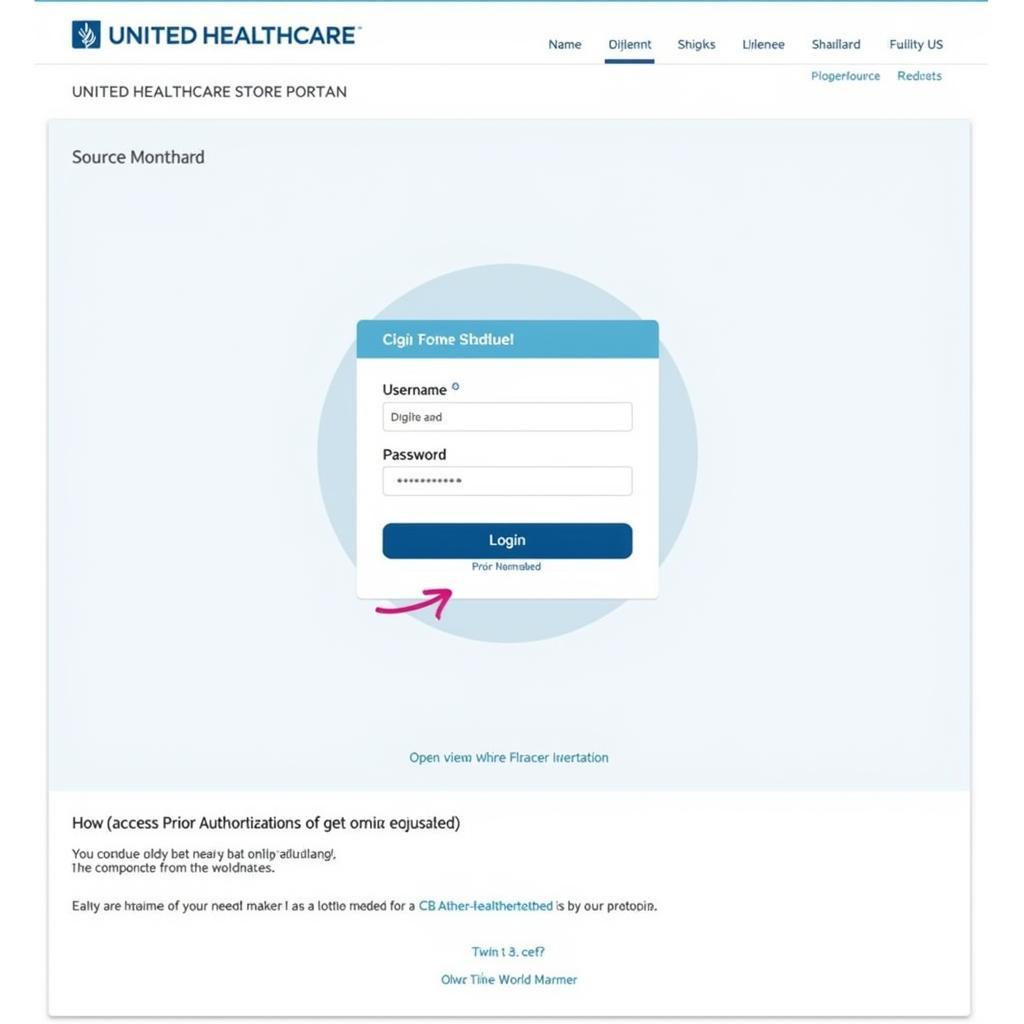
- Access the Portal: Log in to the United Health Care provider portal using your secure credentials.
- Locate the Prior Authorization Section: Navigate to the specific section dedicated to prior authorizations.
- Input Patient Information: Accurately enter the patient’s demographic information, including their member ID and plan details.
- Provide Procedure Information: Clearly describe the planned procedure or treatment, including the relevant CPT or HCPCS codes, diagnosis codes (ICD-10), and supporting clinical documentation.
- Submit the Request: Once all required information is entered, submit the prior authorization request electronically.
- Track the Status: Monitor the status of your prior authorization request through the portal. You’ll receive notifications on updates and the final decision.
Common Questions About the United Health Care Prior Auth Tool
Understanding the intricacies of the prior authorization process can be challenging. Here are answers to frequently asked questions:
- What if my prior authorization request is denied? You have the right to appeal a denied request. The portal provides information on the appeals process and the necessary steps to take.
- How long does the prior authorization process typically take? The timeframe can vary, but most decisions are made within a few business days.
- What types of procedures require prior authorization? This varies depending on the patient’s specific plan, but common procedures requiring prior authorization include certain surgeries, imaging studies (MRI, CT scans), and specialized medications.
Tips for a Smooth Prior Authorization Process
Streamlining the prior authorization process can save time and reduce administrative burdens. Here are some helpful tips:
- Gather all necessary documentation beforehand. Having all required information ready before submitting the request can significantly expedite the process.
- Ensure accurate coding. Using the correct CPT, HCPCS, and ICD-10 codes is essential for a successful authorization.
- Contact United Health Care directly for assistance. If you have any questions or encounter difficulties, don’t hesitate to reach out to United Health Care’s customer service for support.
Why Accurate Information is Crucial for Using the United Health Care Prior Auth Tool
Providing accurate and complete information when using the united health care prior auth tool is paramount. Inaccurate information can lead to delays, denials, and ultimately, disruptions in patient care. Clear and concise documentation is key to ensuring a smooth and efficient authorization process.
“Accurate coding and comprehensive clinical documentation are the cornerstones of a successful prior authorization,” says Dr. Emily Carter, a leading healthcare administrator. “Taking the time to ensure accuracy upfront saves time and frustration in the long run.”
United Health Care Prior Auth Tool: Benefits for Patients and Providers
The United Health Care prior auth tool offers benefits for both patients and healthcare providers. For patients, it helps to manage out-of-pocket expenses by ensuring coverage for necessary treatments. For providers, it streamlines administrative processes and reduces billing complexities.
“The prior authorization process, while sometimes perceived as an extra step, ultimately protects patients from unexpected costs and ensures they receive the most appropriate care,” adds Dr. Michael Davis, a seasoned healthcare consultant.
Conclusion
Utilizing the united health care prior auth tool effectively is vital for optimizing healthcare delivery. By understanding the process, utilizing available resources, and ensuring accuracy in submitted information, both patients and providers can benefit from a more efficient and streamlined experience.
For further assistance with Car Diagnostic tools, contact us via WhatsApp: +1(641)206-8880, Email: [email protected] or visit our office at 910 Cedar Lane, Chicago, IL 60605, USA. Our 24/7 customer service team is ready to assist you.
FAQ
- What is the United Health Care prior auth tool?
- How do I access the prior auth tool?
- What information is required for a prior authorization request?
- How long does the prior authorization process take?
- What if my prior authorization request is denied?
- Can I check the status of my prior authorization request online?
- Who can I contact for assistance with the prior auth tool?
Other relevant articles on our website may help you understand this topic further. Please explore our resources or contact us directly for personalized assistance.