The Esas Tool Palliative Care is a crucial instrument for assessing and managing symptoms in patients receiving palliative care. This article will delve into the importance of the ESAS, its components, and its role in improving the quality of life for individuals facing serious illnesses. We’ll explore how it helps healthcare professionals understand patient needs and tailor care plans accordingly.
What is the Edmonton Symptom Assessment System (ESAS)?
The Edmonton Symptom Assessment System (ESAS) is a simple, validated tool used to assess the severity of nine common symptoms experienced by patients receiving palliative care. These symptoms include pain, tiredness, nausea, depression, anxiety, drowsiness, appetite, well-being, and shortness of breath. The ESAS empowers patients to communicate their symptom burden effectively, which is critical for optimizing their comfort and quality of life. It’s also a vital communication tool between patients, families, and healthcare providers. Early in palliative care, using palliative care symptom assessment tools like the ESAS can significantly improve symptom management and patient outcomes.
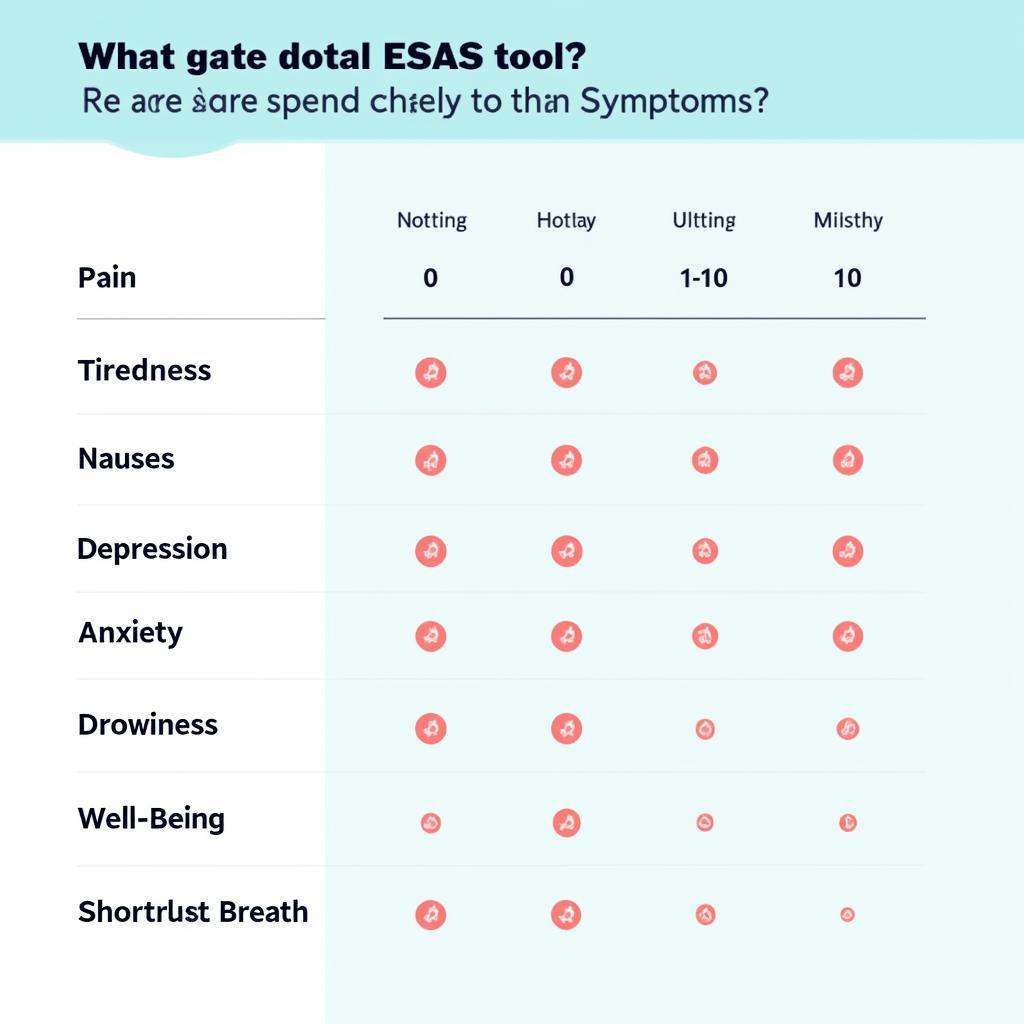 Visual representation of the ESAS tool with its nine symptom categories
Visual representation of the ESAS tool with its nine symptom categories
How Does the ESAS Tool Work?
The ESAS uses a numerical rating scale from 0 to 10 for each symptom, where 0 represents the absence of the symptom and 10 represents the worst possible severity. Patients are asked to rate their symptom experience over the past 24 hours. This simple rating system allows patients to easily express their symptom burden, even if they have difficulty articulating their feelings. The esas tool palliative care allows for regular monitoring, enabling healthcare professionals to track symptom changes and adjust treatment plans as needed. This dynamic approach ensures that care is consistently tailored to the patient’s evolving needs.
Benefits of Using the ESAS Tool in Palliative Care
The ESAS tool offers several advantages in palliative care settings:
- Improved Symptom Management: By regularly assessing symptoms, clinicians can identify and address issues promptly, improving patient comfort and quality of life.
- Enhanced Communication: The ESAS facilitates clear communication between patients, families, and healthcare providers about symptom burden and treatment effectiveness.
- Empowered Patients: The ESAS gives patients a voice in their care, enabling them to actively participate in decision-making. They can express their needs and preferences more directly.
- Easy to Use and Administer: The simplicity of the ESAS makes it accessible to patients with varying cognitive abilities and healthcare providers with diverse backgrounds.
 A patient using the ESAS tool with a doctor’s guidance
A patient using the ESAS tool with a doctor’s guidance
How Does the ESAS Improve Patient Outcomes?
By providing a structured way to assess and track symptoms, the ESAS enables healthcare professionals to make more informed decisions about treatment and care. This can lead to better symptom control, improved quality of life, and greater patient satisfaction. Integrating psychosocial assessment tool for palliative care alongside ESAS further strengthens the holistic approach to patient care.
Addressing Specific Symptoms with ESAS
Each symptom assessed by the ESAS holds significant importance. For example, addressing pain effectively is crucial for enhancing patient comfort. Similarly, managing tiredness and nausea can greatly improve a patient’s ability to participate in daily activities. Recognizing and managing depression and anxiety contributes to overall psychological well-being.
ESAS and Other Palliative Care Assessment Tools
The ESAS is often used in conjunction with other palliative care assessment tools, such as quality of life measures and functional assessments. This comprehensive approach allows for a holistic understanding of the patient’s needs and ensures that care is tailored to address all aspects of their well-being. Understanding the role of palliative care outcome measure tools is crucial for delivering comprehensive and effective palliative care.
 A chart displaying ESAS scores and analysis
A chart displaying ESAS scores and analysis
Conclusion
The ESAS tool palliative care is an invaluable instrument in providing effective and compassionate care to individuals facing serious illnesses. Its simplicity, combined with its ability to capture a wide range of symptoms, makes it a vital component of holistic palliative care. By empowering patients to communicate their needs and enabling healthcare providers to respond effectively, the ESAS contributes significantly to improving the quality of life for those receiving palliative care.
FAQs about ESAS
- How often should the ESAS be administered? The frequency depends on individual patient needs, but it’s often used daily or every few days.
- Who can administer the ESAS? Nurses, doctors, and other trained healthcare professionals can administer the ESAS.
- Is the ESAS used in all palliative care settings? While widely used, it’s not universally implemented in every setting.
- Can family members help patients complete the ESAS? Family members can provide support, but the patient should ideally self-report whenever possible.
- What happens after the ESAS is completed? The healthcare team reviews the results and adjusts the care plan accordingly.
- Is the ESAS translated into other languages? Yes, the ESAS is available in multiple languages.
- Are there any limitations to the ESAS? Like any tool, it has limitations and should be used in conjunction with other assessments.
For any assistance, please contact us via WhatsApp: +1(641)206-8880, Email: [email protected] or visit us at 910 Cedar Lane, Chicago, IL 60605, USA. We have a 24/7 customer support team. You might also be interested in our other articles on psychosocial assessment tools and outcome measure tools for palliative care.

Leave a Reply