Navigating the Iowa Total Care Prior Authorization Lookup Tool can feel daunting. This guide provides a comprehensive overview of the Iowa Total Care prior authorization lookup tool, simplifying the process and offering valuable insights for both patients and healthcare providers.
Understanding the Iowa Total Care Prior Authorization Process
Before delving into the lookup tool, it’s crucial to understand the prior authorization process itself. Prior authorization is a process used by health insurance companies like Iowa Total Care to determine if a specific medication, procedure, or service is medically necessary before it’s covered. This process helps ensure patients receive appropriate care while managing healthcare costs.
Why is Prior Authorization Necessary?
Prior authorization serves several important purposes:
- Ensuring Medical Necessity: It verifies that the requested treatment is indeed necessary and appropriate for the patient’s condition.
- Controlling Costs: By reviewing requests beforehand, insurers can help prevent unnecessary or overly expensive treatments.
- Promoting Safety: The process can help flag potential drug interactions or other safety concerns.
How Does Prior Authorization Work with Iowa Total Care?
With Iowa Total Care, the prior authorization process typically involves the following steps:
- Your doctor identifies the need for a specific medication, procedure, or service.
- Your doctor’s office submits a prior authorization request to Iowa Total Care. This request includes details about your condition and the proposed treatment.
- Iowa Total Care reviews the request. They use established criteria, medical guidelines, and their formulary to determine if the treatment is medically necessary and covered under your plan.
- Iowa Total Care notifies your doctor of their decision. If approved, you can proceed with the treatment. If denied, your doctor may appeal the decision or explore alternative options.
Navigating the Iowa Total Care Prior Authorization Lookup Tool
The Iowa Total Care prior authorization lookup tool is an online resource that allows you to check the status of your prior authorization requests. This can be a valuable tool for both patients and providers, saving time and reducing frustration.
Accessing the Lookup Tool
You can typically access the Iowa Total Care prior authorization lookup tool through their website. Look for a section dedicated to providers or members, where you’ll find links to prior authorization resources.
Using the Lookup Tool
Once you’ve accessed the tool, you’ll likely need to provide some information to look up your request, such as:
- Member ID: Your Iowa Total Care member identification number.
- Date of Birth: Your date of birth.
- Request Date: The date the prior authorization request was submitted.
Understanding the Results
The lookup tool will provide you with the status of your request. This might include:
- Approved: The treatment has been authorized.
- Denied: The treatment has not been authorized. Details about the reason for denial will typically be provided.
- Pending: The request is still under review.
- In Process: The request has been received and is being processed.
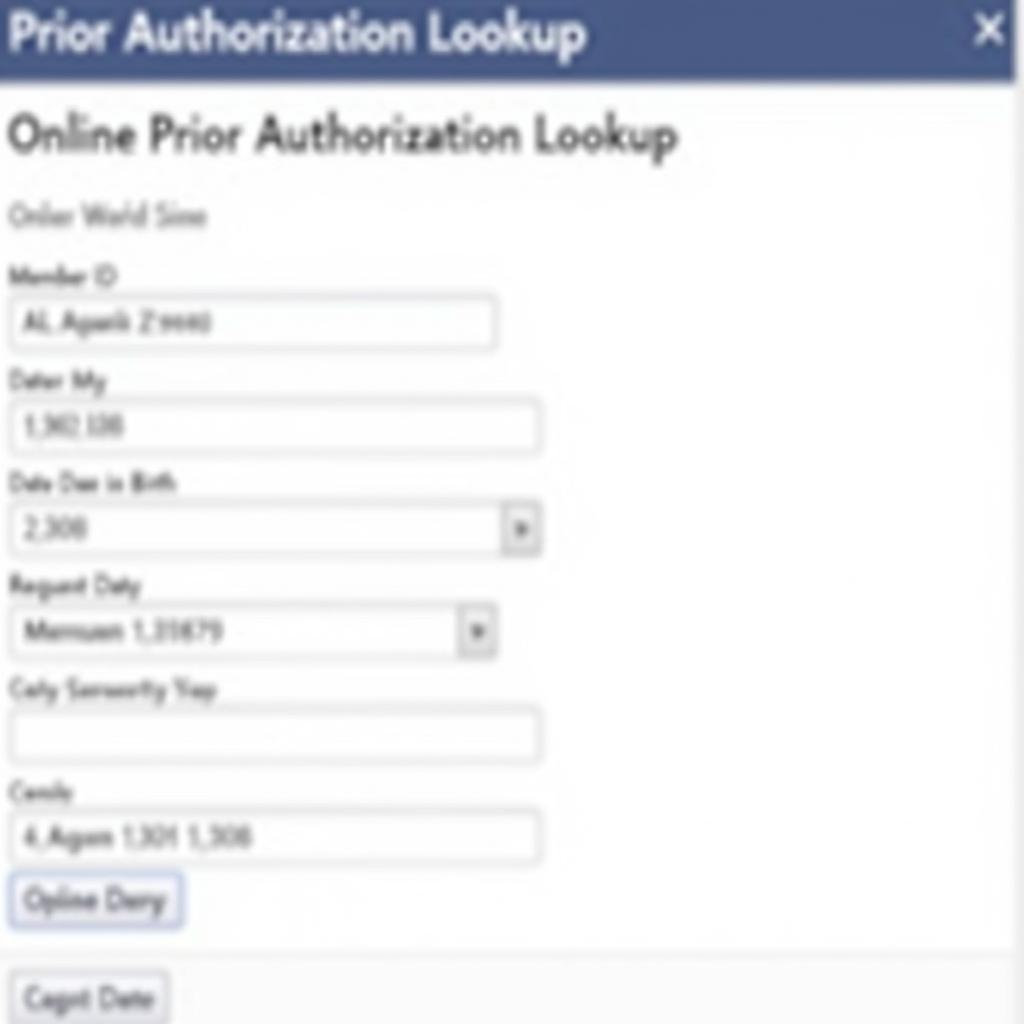 Screenshot of the Iowa Total Care Prior Authorization Lookup Tool
Screenshot of the Iowa Total Care Prior Authorization Lookup Tool
Tips for a Smooth Prior Authorization Process
“A proactive approach to prior authorization can significantly improve the patient experience,” says Dr. Emily Carter, a leading healthcare consultant. “Clear communication between the provider, patient, and insurer is key.” Here are some tips to help streamline the process:
- Work Closely with Your Doctor: Ensure your doctor has all the necessary information about your medical history and current medications.
- Submit Complete and Accurate Information: Accurate and detailed information in the initial request can minimize delays.
- Check the Status Regularly: Use the Iowa Total Care prior authorization lookup tool to track your request and stay informed.
- Contact Iowa Total Care Directly: If you have questions or concerns, don’t hesitate to reach out to Iowa Total Care directly.
Conclusion
The Iowa Total Care prior authorization lookup tool is a valuable resource for managing your healthcare. By understanding the process and utilizing the available tools, you can ensure a smoother experience and timely access to necessary treatments. For further assistance, please consult your healthcare provider or contact Iowa Total Care directly.
FAQ
- What is prior authorization? Prior authorization is the process by which your health insurer approves or denies coverage for a specific medication, procedure, or service.
- How do I access the Iowa Total Care prior authorization lookup tool? You can typically find the lookup tool on the Iowa Total Care website.
- What information do I need to use the lookup tool? You’ll likely need your member ID, date of birth, and the date the request was submitted.
- What does it mean if my request is “pending”? It means Iowa Total Care is still reviewing your request.
- Can I appeal a denied prior authorization? Yes, your doctor can usually appeal a denied request.
- How long does the prior authorization process usually take? The timeframe can vary, but it’s best to contact Iowa Total Care for specific estimates.
- Who should I contact if I have questions about prior authorization? Contact your healthcare provider or Iowa Total Care directly.
Need help with car diagnostics? Contact us via WhatsApp: +1(641)206-8880, Email: [email protected] or visit us at 910 Cedar Lane, Chicago, IL 60605, USA. Our customer service team is available 24/7.

Leave a Reply