The Validation Of The Critical Care Pain Observation Tool (CPOT) is crucial for ensuring accurate pain assessment in critically ill patients who cannot self-report. This article delves into the importance of CPOT validation, its methodology, and its implications for improving pain management in intensive care settings.
Understanding the Need for CPOT Validation
Critically ill patients often experience significant pain due to their underlying conditions, procedures, and interventions. However, many of these patients are unable to communicate their pain levels verbally due to sedation, intubation, or cognitive impairment. This necessitates the use of validated pain assessment tools like the CPOT. The CPOT validation process ensures that the tool reliably and accurately reflects a patient’s pain experience, enabling healthcare professionals to provide appropriate pain management interventions.
Why is Accurate Pain Assessment Important in Critical Care?
Untreated pain in critically ill patients can have serious consequences, including increased physiological stress, prolonged mechanical ventilation, and delayed recovery. Accurate pain assessment is essential for minimizing these risks and improving patient outcomes.
How Does CPOT Validation Contribute to Better Pain Management?
CPOT validation studies provide evidence of the tool’s reliability and validity, giving clinicians confidence in its ability to accurately measure pain. This confidence translates to more effective pain management strategies, leading to improved patient comfort and well-being.
 CPOT Assessment in ICU
CPOT Assessment in ICU
The Methodology of CPOT Validation
CPOT validation involves a rigorous process of evaluating the tool’s psychometric properties. This includes assessing its reliability (consistency of measurement) and validity (accuracy of measurement). Researchers use various statistical methods to determine the tool’s sensitivity, specificity, and predictive value.
Assessing the Reliability of CPOT
Reliability studies examine the consistency of CPOT scores across different raters and over time. High inter-rater reliability ensures that different observers using the CPOT will obtain similar pain scores for the same patient. Good test-retest reliability indicates that the tool produces consistent results when used repeatedly on the same patient over a short period.
Evaluating the Validity of CPOT
Validity studies assess how well the CPOT measures what it intends to measure – pain. This involves comparing CPOT scores with other established pain assessment methods or physiological indicators of pain. Researchers also examine the tool’s ability to discriminate between patients with and without pain.
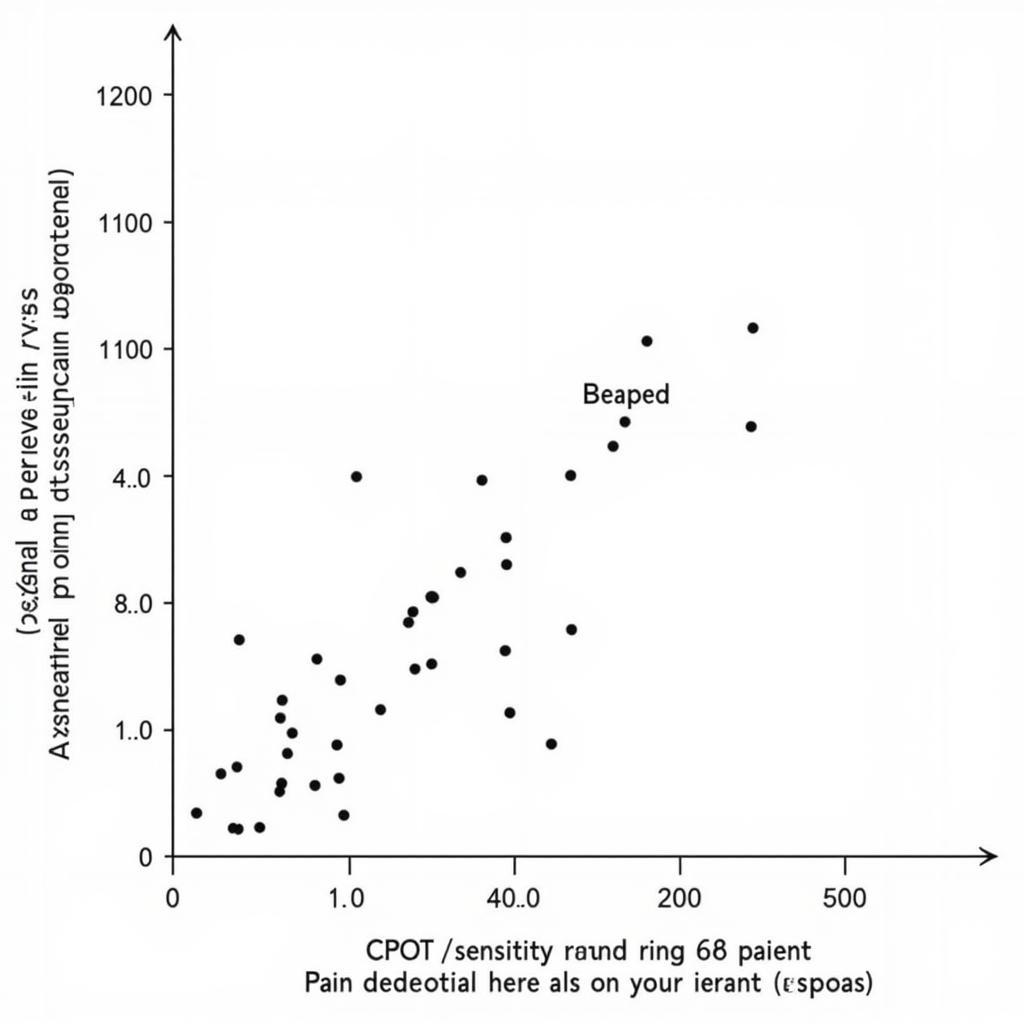 CPOT Validation Study Graph
CPOT Validation Study Graph
Implications of CPOT Validation for Clinical Practice
The validation of the CPOT has significant implications for improving pain management in critical care settings. It provides clinicians with a reliable and valid tool for assessing pain in patients who cannot self-report, enabling them to make informed decisions about pain management interventions.
How CPOT Validation Influences Pain Management Protocols
Validated pain assessment tools like the CPOT are often incorporated into pain management protocols in intensive care units. These protocols provide guidelines for assessing and managing pain in critically ill patients, ensuring that pain is addressed proactively and systematically.
Improving Patient Outcomes Through Validated Pain Assessment
By using a validated tool like the CPOT, clinicians can more accurately assess pain and tailor pain management strategies to individual patient needs. This leads to improved patient comfort, reduced physiological stress, and potentially faster recovery times.
“Accurate pain assessment is the cornerstone of effective pain management in critical care,” says Dr. Emily Carter, a leading expert in critical care medicine. “The validation of the CPOT provides clinicians with a valuable tool for ensuring that no patient suffers needlessly.”
Conclusion
Validation of the Critical Care Pain Observation Tool (CPOT) is paramount for ensuring accurate pain assessment and effective pain management in critically ill patients. By using a validated tool like the CPOT, clinicians can enhance patient comfort, minimize suffering, and contribute to better overall outcomes. Further research and refinement of pain assessment tools will continue to advance pain management practices in critical care.
“The ongoing validation and refinement of tools like the CPOT demonstrate the commitment of the medical community to providing the best possible care for critically ill patients,” adds Dr. Michael Davis, a renowned researcher in pain management.
FAQ
- What is the CPOT?
- How is the CPOT used?
- What are the benefits of using a validated pain assessment tool?
- How often should the CPOT be used?
- Who can use the CPOT?
- What are the limitations of the CPOT?
- Where can I find more information on CPOT validation studies?
Common Scenarios and Questions:
- How to differentiate between agitation and pain using CPOT?
- What to do when CPOT scores are consistently high?
- How to adapt CPOT for patients with specific conditions (e.g., neuromuscular disorders)?
Further Reading and Resources:
- Pain Management in the ICU: A Comprehensive Guide
- Understanding the Validity and Reliability of Pain Assessment Tools
Need assistance? Contact us via WhatsApp: +1(641)206-8880, Email: [email protected] or visit our office at 910 Cedar Lane, Chicago, IL 60605, USA. Our customer support team is available 24/7.

Leave a Reply